“Bacterial Intrusion: Unraveling the Gut-Eye Connection in Genetic Retinal Diseases”
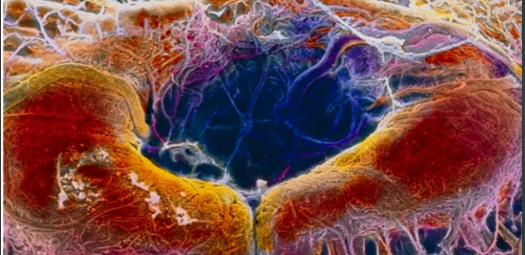
Emerging research challenges the Bacterial Intrusion conventional belief that eye diseases are solely genetic, suggesting a potential link between bacteria escaping the gut and retinal disorders. Typically, the eyes are considered protected by a tissue layer impervious to bacterial penetration, making the recent findings unexpected and groundbreaking. This paradigm-shifting study, published in Cell on February 26, could transform our understanding of the causes of certain eye conditions and open new avenues for treatment.
Bacterial Intrusion
Inherited retinal diseases, such as retinitis pigmentosa, affect approximately 5.5 million people globally. Among the leading causes of these conditions are mutations in the Crumbs homolog 1 (CRB1) gene, which can lead to blindness. Previous research had hinted at the presence of bacteria in the eyes, contrary to the long-standing belief that the eyes are sterile environments. This prompted scientists to explore whether bacteria play a role in retinal diseases.
The study, led by ophthalmologist Richard Lee from University College London and published in Cell, focused on understanding the impact of CRB1 mutations. The research uncovered a dual role of CRB1 mutations, weakening both the linkages between cells lining the colon and the protective barrier around the eyes. This revelation led the researchers to hypothesize that bacteria escaping the gut could contribute to retinal diseases.
To test their hypothesis, the team created Crb1-mutant mice with reduced bacterial levels. Remarkably, these mice did not exhibit distorted cell layers in the retina, unlike their counterparts with typical gut flora. This indicated a direct connection between gut bacteria and the development of retinal disorders in the presence of CRB1 mutations.
Further experimentation involved treating the mutant mice with antibiotics, resulting in reduced eye damage. This suggested a potential therapeutic approach for individuals with CRB1 mutations—administering antibiotics or anti-inflammatory drugs to counteract the effects of bacteria. If validated, such treatments could significantly improve the lives of families affected by these genetic conditions.
However, neurobiologist Jeremy Kay from Duke University urges caution and skepticism, emphasizing the complexity of the picture. While the study presents a novel idea, Kay cautions against assuming an easy solution for patients with CRB1 mutations. The specific mice used in the study typically take years to fully develop Crb1-associated eye diseases, raising questions about the direct applicability of the results to humans.
Moreover, Kay questions whether the bacteria actually reach the eyes in sufficient quantities to have a significant impact. The study focused on a specific type of bacteria in mice, and extrapolating these findings to human cases remains uncertain. Kay argues that even if gut bacteria contribute to eye infections, it would be logical to assume similar infections in other parts of the body, a phenomenon not yet observed in people with CRB1 mutations.
The translation of these findings to human treatments remains a significant challenge. Nevertheless, the study opens up intriguing possibilities for investigating the role of gut bacteria in retinal diseases and exploring potential interventions. Lee suggests that the bacterial translocation from the gut could preferentially infect specific sites, a phenomenon not fully understood by scientists.
In light of these findings, Lee encourages cautious exploration, stating that attempting antibiotics in patients may be a reasonable approach. However, he acknowledges the broader genetic changes caused by CRB1 mutations, implying that antibiotics might address retinal damage but may not reverse or cure the genetic alterations.
The study introduces a novel perspective on the interplay between genetics and microbiology in the context of eye diseases. If further research confirms the role of gut bacteria in retinal disorders, it could revolutionize treatment strategies, offering hope to individuals affected by these genetic conditions. As the scientific community delves deeper into this uncharted territory, the potential for groundbreaking advancements in ophthalmology and genetic medicine looms on the horizon.