The proposed Assisted Dying Bill in Scotland has reignited a contentious debate over the ethical, legal, and practical implications of allowing terminally ill individuals the option to end their lives with medical assistance. Supporters of the legislation argue that it would alleviate suffering for those facing terminal illnesses, providing them with a compassionate choice to die on their own terms. However, opponents express concerns about the potential for coercion and the erosion of safeguards meant to protect vulnerable individuals.
Dying Bill
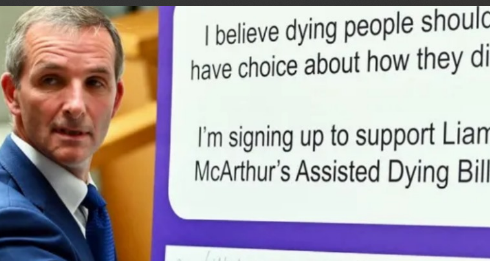
The bill, introduced by Lib Dem MSP Liam McArthur, aims to address the complex issue of assisted dying by establishing stringent criteria for eligibility. Under the proposed legislation, individuals with terminal illnesses would be able to request medical assistance to end their lives only if they meet specific conditions. These conditions include being mentally competent to make such a decision, having a terminal illness that is advanced and progressive, and being a resident of Scotland for at least 12 months. Additionally, the patient must administer the life-ending medication themselves, ensuring autonomy and control over the process.
Proponents of the bill argue that it offers a compassionate option for individuals facing unbearable suffering at the end of their lives. They emphasize the importance of respecting patients’ autonomy and dignity, allowing them to make informed decisions about their own deaths. Mandie Malcolm, a terminally ill patient, shares her concerns about the possibility of experiencing unbearable pain and suffering in her final days. For her, the option of assisted dying provides a sense of relief and peace of mind, knowing that she has control over her own destiny.
However, opponents of the bill raise valid concerns about the potential risks and unintended consequences of legalizing assisted dying. Dr. Fiona MacCormick, representing the Association for Palliative Medicine, warns against the normalization of suicide and the potential for coercion in vulnerable populations. She highlights the importance of palliative care as an alternative approach to alleviating suffering at the end of life, emphasizing the need for greater investment in supportive services and pain management.
Moreover, critics argue that the bill’s safeguards may not be sufficient to prevent abuse or protect individuals from undue pressure to end their lives prematurely. Audrey Birt, a terminally ill patient receiving palliative care, expresses her reservations about the bill, fearing that some patients may feel compelled to choose assisted dying due to societal expectations or perceptions of being a burden. She advocates for increased funding for palliative care services as a more compassionate and holistic approach to end-of-life care.
The proposed Assisted Dying Bill also faces opposition from religious institutions and medical professionals who object to the moral and ethical implications of deliberately ending a person’s life. The Church of Scotland, the Catholic Church in Scotland, and the Scottish Association of Mosques have all voiced their opposition to the bill, citing concerns about the sanctity of life and the potential for abuse.
Despite the controversy surrounding the bill, public opinion appears to be divided on the issue of assisted dying. A recent poll conducted by Opinium Research found that 78% of respondents in Scotland supported making assisted dying legal, indicating widespread public support for the proposed legislation. However, the bill’s fate ultimately lies in the hands of Scottish lawmakers, who must carefully consider the moral, ethical, and practical implications of such a significant legislative change.
In conclusion, the Assisted Dying Bill in Scotland has sparked a heated debate over the rights of terminally ill individuals to choose how and when they die. While supporters argue that it offers a compassionate option for those facing unbearable suffering, opponents raise concerns about coercion, safeguards, and the sanctity of life. As the bill moves forward for debate and potential vote, lawmakers must carefully weigh these competing interests and consider the profound implications for end-of-life care in Scotland.